70 years old male with Altered sensorium
12th Jan 2022
This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
Name: K. Thanmai reddy
Roll.no:65
Batch :2017
A 70 year old male patient who is daily wage labourer by occupation was brought to the casualty on 6th jan with the chief complaints of altered sensorium since five days. Burning sensation in oral cavity, difficulty in swallowing, shortness of breath and productive cough since 25 days.
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 20days ago when he went on a sudden alcohol binge for a couple of days following which he developed cough assosciated with sputum (scanty, non foul smelling, non blood tinged) and
Shortness of breath which was initially Class 2( slight limitation of physical activity) but gradually progressed to class 4(SOB at rest, unable to carry physical activity without discomfort).(NYHA)
He also had burning sensation of the oral cavity since 25 days and pain on swallowing for which he was treated symptomatically by chlorhexidine mouth wash and mouthguard gel
Following these complaints, the patient was taken to a nearby Government hospital, where he was treated symptomatically.
Then the patient was shifted to another local hospital where a chest X Ray was done and he was told he has viral pneumonia of the right lung.
Five days back(6th of jan) patient was brought to our hospital by his wife who said that she noticed a change in his responsiveness and slurring of speech that began 3 days ago. The patient presented to the casuality ward with some drowsiness, but he was arousable.
On examination of his oral cavity, multiple erythematous lesions are seen over his hard palate
PAST HISTORY :
No similar complaints in the past.
Not a known case Diabetes mellitus
Hypertension
TB,
Asthma,
Epilepsy,
CAD.
H/o Surgery and blood transfusion:there history of transfusion of two units of FFP
Central line for dialysis on 7th jan
FAMILY HISTORY :
No history of similar illnesses among immediate family members.
No significant family history.
The patient lost his first wife to an unknown illness 30 years ago. He has 2 daughters with his second wife.
PERSONAL HISTORY:
Diet: Mixed
Appetite: decreased recently
Sleep:Adequate
Bowel and bladder: Decreased urine output
No known drug allergies
He consumes 150ml of Alcohol every other day, his last intake was 25 days back.
Tobacco usage since 30 years .
GENERAL EXAMINATION :
Patient is conscious, not coherant or cooperative, not oriented to time, place and he is drowsy,appears confused and irritated.
Moderately built and nourished.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema.
VITALS:
PR: 87 bpm
BP: 120/70 mmHg
RR: 24 cpm(tachypnic)
SpO2: 98% with 4L of O2
Temperature: febrile on arrival
GRBS: 229mg/dl
CNS: GCS: E4V4M6
Cranial nerve examination intact
Speech slurred
Sensory system- sensitive to pain, touch , vibration and temperature.
Motor system : Right. Left
Power- UL 5/5 5/5
LL 5/5 5/5
Neck ,trunk power normal
Tone- UL Normal Normal
LL Normal Normal
Reflexes-
Superficial reflexes - Intact
Plantar flexion flexion
Deep tendon reflexes -
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle ++ ++
Gait- Normal
Cerebellar system - intact
Respiratory system: inspection:
trachea central in position.
On auscultation:bilateral air entry present
B/L Crepititions heard, NVB
On percussion:dullness on right upper lobe,
CVS: S1, S2 heard, no murmurs
Abdominal examination:
Inspection:
Shape of abdomen -scaphoid
Position of Umbilicus- Central and inverted
All Quadrants of abdomen moving with respiration.
No visible scars and sinuses.
Hernial orifices free
No visible pulsations.
Palpation :
Soft
No tenderness
LIVER - Not Palpable
SPLEEN- Not Palpable
Percussion :
NO SHIFTING DULLNESS
NO FLUID THRILL
Auscultation :
Bowel sounds heard.
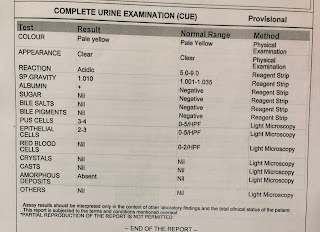
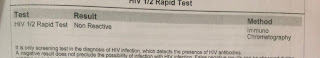
Investigations:
Chest X-ray
Uric acid:
Provisional diagnosis:
altered sensorium secondary to uremic encephalopathy, viral pneumonia with acute kidney injury secondary to sepsis.
TREATMENT:
-intravenous fluid ( normal saline,ringer lactate
- Ryle tube feeds 100 ml milk 2 nd hourly
50 ml water hourly
-Head end elevation
- O2 inhalation to maintain spo2 >94%
- Inj.AUGMENTIN 1.2 gm IV BD
-Inj.HYDROCORTISONE 100mg IV/STAT
-tab.AZITHROMYCIN 500mg RT/OD
-tab.MONTEK-LC RT/OD
-tab.ACEBROPHYLLINE RT/OD
-NEB with BUDECORT -12th hourly.
IPRAVENT -4th hourly
MUCOMIST-2nd hourly
-SYP AMBRONYL 15ml RT/TID
- temperature charting
-GRBS- 6 th hourly
- Inj.LASIX 40mg IV/ BD( if BP > 110 mm Hg)
-Inj.PIPTAZ 45 mg IV/ STAT
-MUCOPAIN gel
- BETADINE gargles T


















Comments
Post a Comment