46 year old patient with emphysematous pyelonephritis
Short case:FINAL MBBS PRATICAL EXAMINATION:
June 10' 2022
A 46yr old male patient with emphysematous pyelonephritis
This is an online E-log book to discuss our patient
de-identified health data shared after taking his/ her
guardians sign informed consent.
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aim to solve those patient clinical problem with collective current best evidence based inputs.
This E-log also reflects my patient centered online learning portfolio.
Your valuable inputs on comment box is welcome.
Name: K. Thanmai
Roll no :65
Batch : 2017
Hall ticket : 1701006087
CASE PRESENTATION :
A 46 year old male came with chief complaints of:
Burning micturition present since 10 days
Vomiting since 2 days ( 3 - 4 episode)
Giddiness and deviation of mouth since 1 day
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 10years back,
he complained of polyuria for which he was diagnosed
with Type 2 diabetes mellitus he was started on OHAs.
3years back OHAs were converted to insulin.
2 days back, he developed vomiting , containing food
particles and non bilious. He also complained of
deviation of mouth and giddiness 1 day
His GRBS was also recorded high , for which he was
given NPH 10 IU and HAI 10 IU
3 years back , he underwent cataract surgery.
1 year back, he had h/o small injury on leg which
gradually progressed to non healing ulcer extending
upto below knee eventually ended with below knee
amputation due to development of wet gangrene.
Not a k/c/o HTN/Epilepsy/TB/BA/Thyroid disorder/CAD/CVD
PERSONAL HISTORY:
Diet - Mixed
Appetite- normal
Sleep- Adequate
Bowel and bladder- Regular
Micturition- burning micturition present
Habits/Addiction:
Alcohol-
Not consuming alcohol since 1 yr.
Previously (1yr back) Consumption of
alcohol, about 90mlwhiskey almost daily.
Also 1month on&off consumption pattern was
previously present.
FAMILY HISTORY:
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
Reflexes: (Biceps/Triceps/Knee/Ankle/Plantar)Normal
Power: Normal(5/5) in both Upper and Lower limbs
Tone: Normal in both Upper and Lower limbs
No meningeal signs
Investigations:
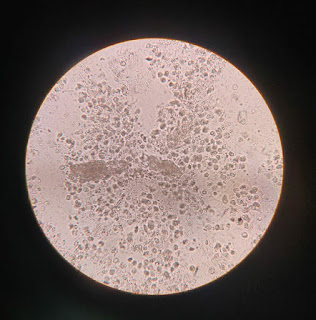
BACTERIAL CULTURE REPORT:
PROVISIONAL DIAGNOSIS:

















Comments
Post a Comment